5005 S. Cooper St.
Suite 250
Arlington, TX 76017
Prostate Cancer Is Scary
We Are Warriors!
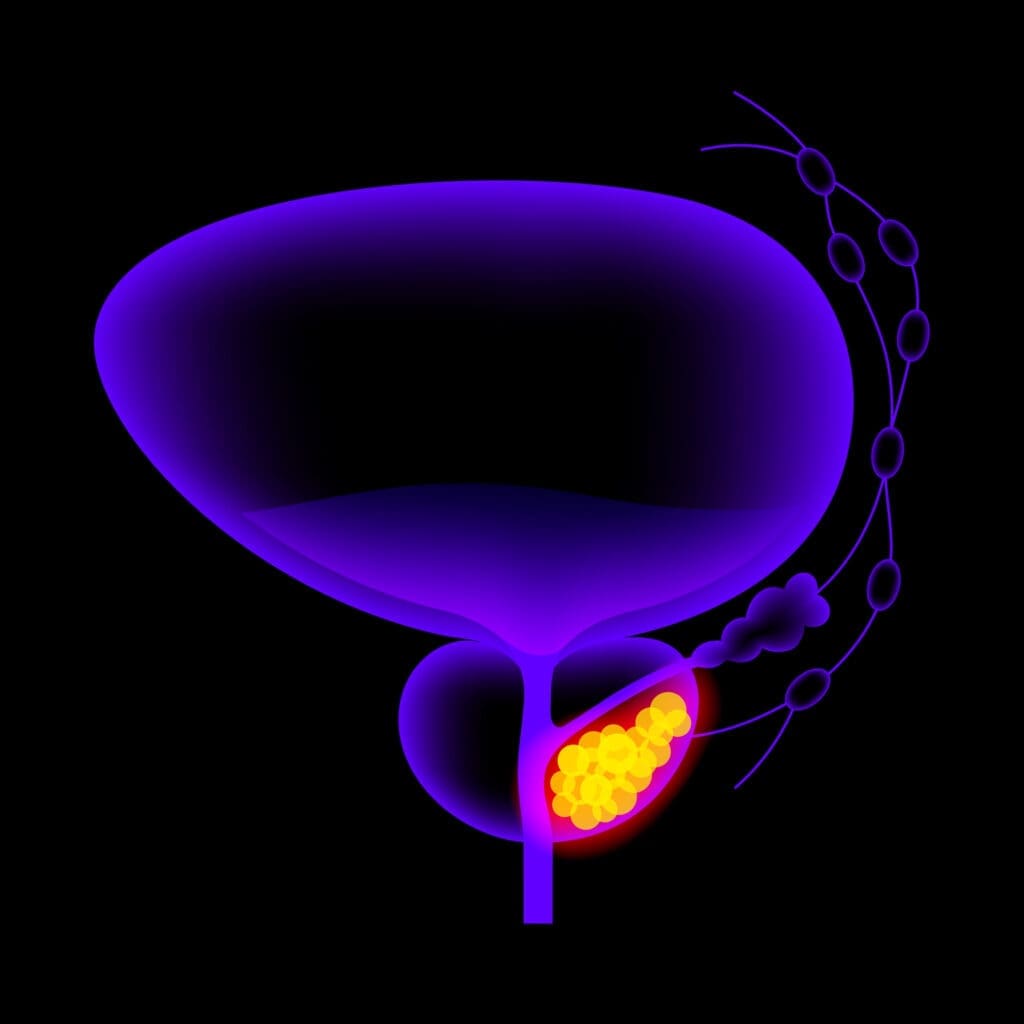
What is prostate cancer?
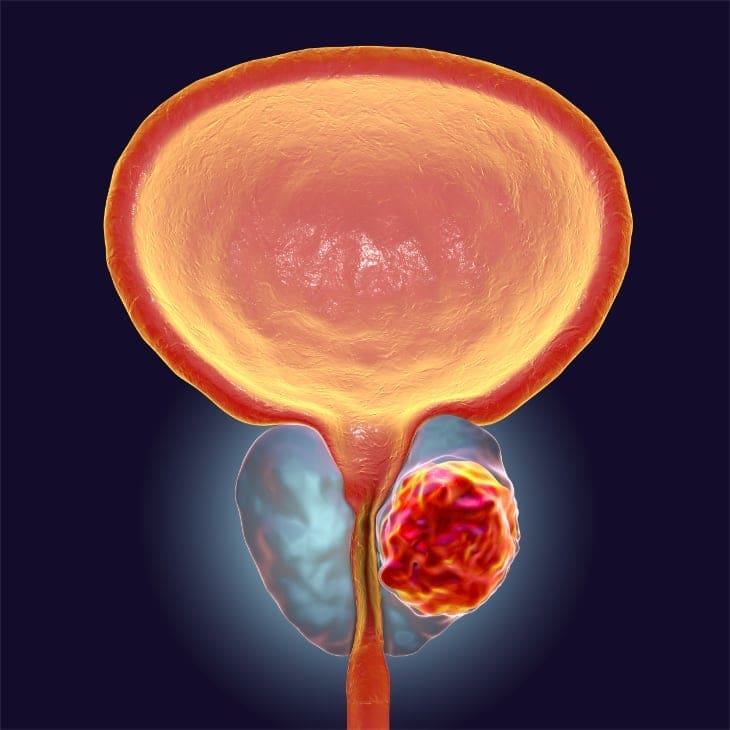
Located deep inside the groin between the base of the penis and the rectum, the golf-ball-sized prostate gland, along with the seminal vesicles behind the prostate, produces seminal fluid which mixes with sperm from the testes to help sperm travel. Prostate cancer occurs when healthy cells in the prostate begin to mutate and grow out of control. When the abnormal cells clump together, they form a cancerous tumor. Researchers still don’t have all the answers about what triggers changes to prostate cells, but know that genetics, family history, ethnicity, a high-fat diet and obesity are all risk factors.
How is prostate cancer diagnosed?
There are several steps involved in screening for and diagnosing prostate cancer, including PSA testing, digital rectal exam (DRE), and biopsy.
PSA Testing
A simple blood test to detect the presence of prostate-antigen antibody (PSA)—a protein produced by the prostate—is the first step toward monitoring the health of the prostate. The first PSA test provides patients and physicians with an important baseline that can be monitored over time to track a suspicious rise in level. Generally, levels measuring less than 2.5 are considered within normal range, but a rise in PSA greater than 0.35 per year or a doubling within a year raises suspicions about cancer.
Digital Rectal Exam
Since the prostate is not easily visible, a digital rectal exam (DRE) allows the physician to feel the prostate by inserting a gloved finger into the rectum. If the prostate feels hard, lumpy or has any abnormal areas, it could be a warning sign for prostate cancer. While a DRE is often a source of apprehension for many men, the exam takes only a few seconds and causes mild discomfort. A DRE test, along with PSA testing, is an important part of regular prostate cancer screening.

Biopsy
Although results from a PSA test and DRE are the first indicators that prostate cancer may be present, a transrectal ultrasound (TRUS) guided biopsy or magnetic resonance imaging (MRI) fusion-guided biopsy are conducted to confirm a diagnosis.
TRUS-Guided Biopsy
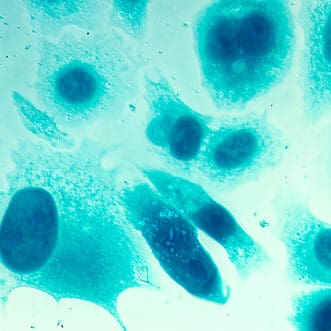
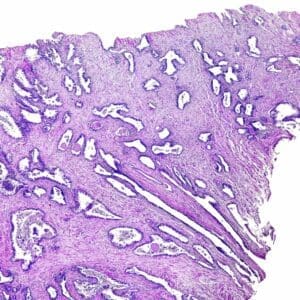
Under local anesthetic, a lubricated ultrasound probe is placed in the rectum allowing the physician to see the shape and size of the prostate—along with any apparent abnormalities or shadows that may indicate cancer. After the prostate gland is injected with numbing anesthetic, slim needles are used to gather samples from several zones of the prostate including suspicious-looking areas (although not all prostate cancers are visible). The collected tissue samples are sent to a pathologist who will examine them to determine if cancer is present.
Magnetic Resonance Imaging (MRI)
Magnetic Resonance Imaging (MRI) has been used for many years to evaluate soft tissue, but has only become mainstream for prostate imaging over the last seven to 10 years. Because the prostate is a very dense organ, it was very difficult to visualize with previous MRI machines. Now newer, more powerful magnets—the 3 Tesla (3T)—have significantly improved the images collected.
In 2012, the PI-RADS (v.1) imaging grading system was introduced. This grading system enables radiologists and urologists to grade abnormal areas in the prostate. The PI-RADS scale ranges from 1 to 5 with 5 being the highest rating and indicating areas most likely to harbor a focus of intermediate or high-grade prostate cancer. While the MRI is roughly 80 percent accurate in finding intermediate to high- grade prostate cancer, it often misses lower-grade prostate cancer. This is currently rarely an issue, though, as many of these men are candidates for active surveillance to follow these low-risk cancers without treatment.Not all MRIs are built the same, so it is extremely important to discuss your MRI with your urologist. Urology Partners currently recommends Gateway Imaging in Arlington because they have the MRI and software specifications to produce high-quality images that are compatible with our inVivo Uronav fusion biopsy software system.
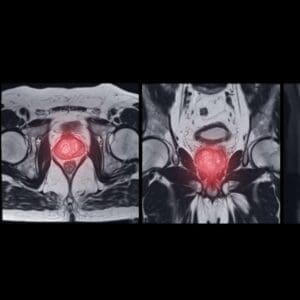
MRI Fusion-Guided Biopsy
TRUS-guided biopsies don’t always deliver definitive answers. There have been many cases where men with PSA levels of 20 or 30 have undergone several biopsies that repeatedly come back negative. Their cancer could not be located due to limitations of the TRUS technology. In an effort to get a clearer picture of the prostate and suspicious areas, many men have a prostate MRI before their biopsy, or as a follow-up after a negative biopsy with a persistently elevated PSA.Not all prostate cancer is the same.
Cancer Grading
Grading refers to the way cancer looks under a microscope. When abnormal-looking cancer cells are found, the pathologist ranks them according to the degree of visible change. While early-stage or low-grade cancer cells may look only slightly different from healthy cells, high-grade cancer cells look dramatically different. Each of the tissue samples collected during a biopsy is assigned a number according to the Gleason Grade from 3 to 5 if cancer is present. The number 3 indicates the “least aggressive” grade of prostate cancer, while the number 5 represents the “most aggressive” grade of the disease.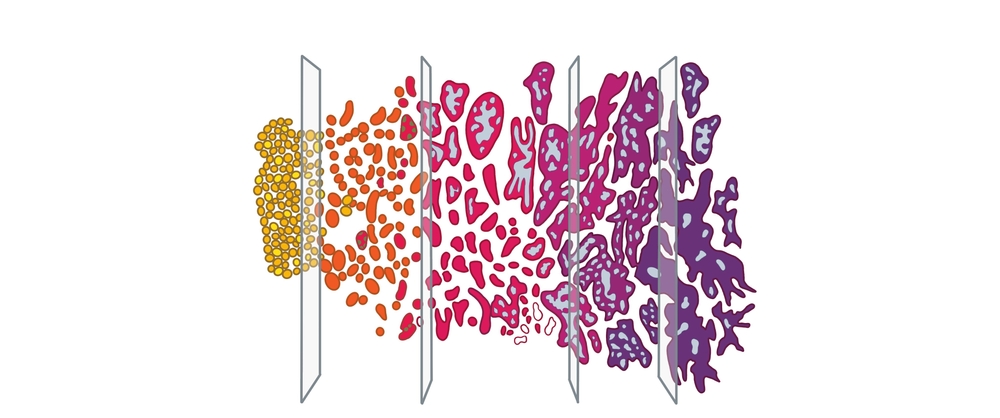
Cancer Staging
There are actually two types of staging for prostate cancer—the clinical and pathologic staging. Clinical staging is the doctor’s best estimate regarding the extent of the prostate cancer based on the results of a physical exam, digital rectal exam (DRE), lab tests, prostate biopsy and imaging tests. Pathologic staging is based on the examination of tissue removed during surgery. Pathologic staging is likely to be more accurate than clinical staging because it enables physicians to get firsthand knowledge about the extent of the cancer.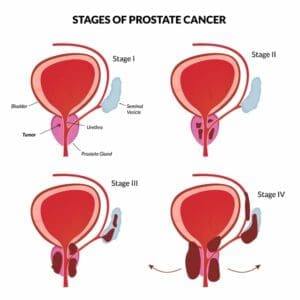
Pathological Staging
Staging refers to how much the cancer has grown and spread. Is it confined locally within the prostate? Has it spread beyond the prostate and into the lymph nodes, or metastasized to the bones? In cases where the Gleason score is on the high side, additional tests such as an MRI, CT scan or bone scan will be conducted to help stage the prostate cancer more precisely. Based on these reports, the American Joint Committee on Cancer TNM (Tumor, Node, Metastasis) Staging System is used to describe how far the cancer has spread. The TNM system is based on three important pieces of information:T1a – cancer found in 5% of TURP specimens
T1b – cancer found in more than 5% of TURP specimens
T1c – cancer found on prostate needle biopsy only because of elevated PSA
T2a – cancer found in less than 50% of one side of the prostate
T2b – cancer found in more than 50% of one side of the prostate
T2c – cancer found in both sides of the prostate
T3a – cancer has spread outside the prostate, but not to seminal vesicles
T3b – cancer has spread to the seminal vesicles
T4 – cancer has grown into the nearby tissues such as bladder or pelvic sidewall
Nx – lymph nodes have not been assessed for cancer
N0 – no cancer in nearby lymph nodes
N1 – cancer has spread to nearby lymph nodes
Mx – it is unknown if cancer has spread to distant sites
M0 – cancer has not spread to distant sites
M1 – cancer has spread to distant sites
M1a – cancer has spread to distant lymph nodes
M1b- cancer has spread to bones
M1c – cancer has spread to distant organs
Health Navigator
- Harrison “Mitch” Abrahams, MD
- Jeffrey Charles Applewhite, MD
- Jerry Barker, MD, DABR, FACR
- Paul Benson, MD
- Richard Bevan-Thomas, MD
- Keith D. Bloom, MD
- Tracy Cannon-Smith, MD, FMS
- Paul Chan, MD
- Kara Choate, MD
- Lira Chowdhury, DO, FACOS
- Weber Chuang, MD
- Adam Cole, MD, FS
- M. Patrick Collini, MD
- Zachary Compton, MD
- Adam Hollander, MD
- Patrick A. Huddleston, MD
- Justin Tabor Lee, MD
- Wendy Leng, MD, FPMRS
- Alexander Mackay, MD
- Tony Mammen, MD
- F.H. “Trey” Moore, MD
- Geofrey Nuss, MD
- Christoper Pace, MD
- Jason Poteet, MD
- Andrew Y. Sun, MD
- Scott Thurman, MD
- James Clifton Vestal, MD, FACS
- Keith Waguespack, MD
- Diane C. West, MD
- Keith Xavier, MD, FPMRS
Related News & Information
Treatment Depends on Several Factors
While every individual’s cancer case is unique, Urology Partners follows treatment guidelines established by the National Comprehensive Cancer Network (NCCN). The NCCN system takes Gleason Grade, cancer stage, PSA and the presence or absence of lymph node and bone involvement into consideration before recommending treatment based on a man’s risk category—very low risk, low risk, intermediate risk or high risk.

Active Surveillance
Thirty years ago, about one-third of men diagnosed with prostate cancer already had metastatic cancer that had spread to their bones or lymph nodes. Now that number is below 10 percent because more men are diagnosed in the very early stages of prostate cancer. Not all prostate cancer behaves the same, not all men need immediate treatment. Rather than undergoing surgery or radiation treatments immediately after a prostate cancer diagnosis, some men can be actively monitored for a period of time. This monitoring is known as active surveillance.
During active surveillance, men have a PSA test every six months, and see their urologist to determine if there have been any significant changes. Research shows that men who are good candidates for active surveillance—and who opt to participate in it as a first step in their treatment—have outcomes that are just as good as men who undergo radiation or surgery right away. Biopsies and prostate MRIs are routinely recommended as a follow-up measure in the years after the original diagnosis to ensure there is no evidence of higher-grade cancer that may require treatment.
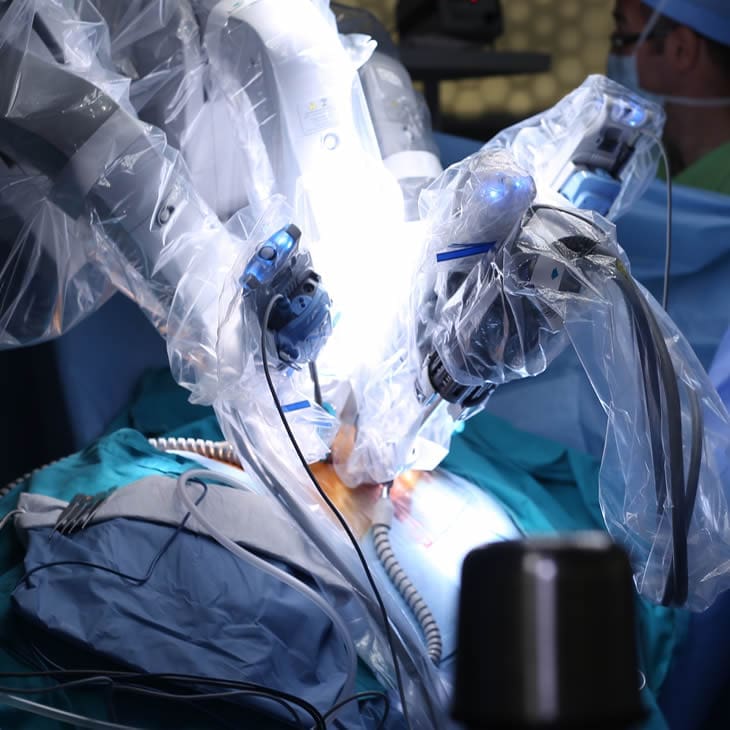
Robot-Assisted Laparoscopic Radical Prostatectomy
The surgical removal of the entire prostate gland and seminal vesicles is a treatment option for men with intermediate or high-risk cancer that has not spread beyond the prostate. Unlike open radical prostatectomy that requires a large incision in the abdomen, Urology Partners surgeons use the da Vinci Surgical® System to perform a robot-assisted laparoscopic radical prostatectomy.
The procedure requires only small abdominal incisions to accommodate a slim robotic arm controlled by the surgeon. A high-definition camera provides a clear, magnified view of the patient’s anatomy, and precision tools give the surgeon the delicate control needed to remove cancerous tissue without damaging surrounding nerves.
In experienced hands, patients who undergo a robot-assisted prostatectomy lose less blood, heal more quickly, have a shorter hospital stay and return to normal activities more quickly.
Today, survivor rates 15 years post-prostatectomy are as high as 93 percent. Urology Partners has some of the most experienced robotic surgeons in the United States—skilled surgeons who have been performing robotic surgery since its early inception in 2002.

Intensity-Modulated Radiation Therapy
Intensity-modulated radiation therapy (IMRT) kills cancerous tissue by damaging its DNA and halting its growth cycle. Using state-of-the-art technology, this targeted approach pinpoints the exact location and shape of the prostate cancer tumor to deliver a very precise dose of radiation. The focused radiation destroys cancer cells while avoiding adjacent healthy tissue and organs—including the bladder and rectum. With no incision, no pain and no recovery time, most men can go about their daily lives with minimal disruption. Treatment sessions last minutes, not hours.
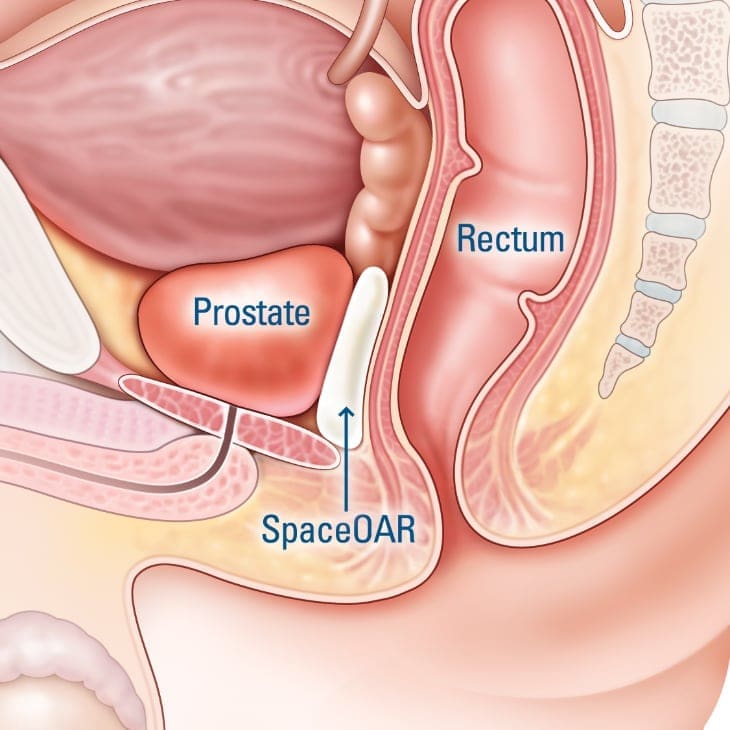
SpaceOAR & Barrigel
Radiation therapy is very effective in treating advanced prostate cancer. At Urology Partners, we help men take extra precautions to protect the rectum and prevent unpleasant post-radiation side effects.
Men can choose to have a soft, absorbable gel—either SpaceOAR or Barrigel—carefully injected into the narrow space between the prostate and rectum before their first radiation treatment. Both gels provide a cushioned barrier that helps shield the rectum from radiation and reduce post-radiation side effects such as rectal pain and bleeding, chronic diarrhea, urinary urgency and leakage, and erectile dysfunction.
Performed under local anesthesia, most men only experience a pin prick or slight pressure during the injection, and generally do not feel any prolonged discomfort during or after the procedure. Patients are able resume their normal activities soon afterward. SpaceOAR and Barrigel are fully absorbed in just a little over six months.

Cryosurgery
This minimally invasive alternative to other surgical and radiation treatments is an option for men with localized prostate cancer. Slim cryoprobes deliver cycles of extremely cold and warm temperatures that repeatedly freeze and thaw cancerous cells within and around the prostate gland—ultimately destroying them.
Ultrasound technology guides the strategic placement of the probes into and around the prostate while minimizing damage to surrounding tissue. With two or more cycles, cancerous cells are destroyed, while the other tissue is either absorbed by the body or remains as scar tissue. Because the procedure is relatively short (usually 1 to 1.5 hours), men experience fewer side effects and enjoy faster recovery. Unlike radiation therapy or a radical prostatectomy, cryosurgery can be repeated if necessary.
HIFU
High-intensity focused ultrasound (HIFU) is another non-invasive therapeutic technique used to treat prostate cancer. It utilizes ultrasound waves to generate heat that precisely targets and destroys cancerous tissues within the prostate. During the procedure, a rectal probe is inserted to emit focused ultrasound beams into the prostate and raise the temperature to about 80 to 100 degrees Celsius, effectively obliterating the cancerous cells while sparing the surrounding healthy tissues. The accuracy of HIFU minimizes the damage to nearby structures, reducing the risk of common side effects associated with other prostate cancer treatments, such as urinary incontinence and sexual dysfunction. With real-time imaging guidance, the surgeon can continuously monitor and control the treatment, ensuring the desired therapeutic outcome while minimizing collateral damage. HIFU is routinely used for patients with localized prostate cancer and primarily for patients with cancer on only one side of the prostate.
Nanoknife
This newer, minimally invasive treatment uses irreversible electroporation (IRE) technology to target and treat prostate cancer cells. Under image guidance, typically ultrasound or CT, needle-like electrodes are inserted into and around the cancerous tissue. Once in position, the Nanoknife delivers a series of short, intense electric pulses to create precise and irreversible nanopores in the cell membranes. This leads to cell death without the use of thermal energy—minimizing collateral damage to surrounding tissues. This method helps preserve crucial structures like the urethra and neurovascular bundles to reduce urinary incontinence, erectile dysfunction and other common side effects associated with other prostate cancer treatments. Similar to HIFU, this treatment is also routinely used for men with localized cancer.
We Are Your Prostate Cancer Specialists
Call for an Appointment
Prostate Cancer Survivor Paul Moseley Shares His Gratitude for Life
Paul Moseley remembers the day he learned he had prostate cancer in November 2013. “I don’t scare easily, but I was shook,” he admits. “You think you have this big distance ahead of you, and it turns out it could be really short.” The long-time Fort Worth Star-Telegram news photographer,

