5005 S. Cooper St.
Suite 250
Arlington, TX 76017
Anxious About Your PSA Level?
Men often worry that an elevated PSA means they may have prostate cancer. This isn’t always the case. PSA levels can fluctuate. While there’s no true cutoff for PSA, a level above 2.5 mg/ml should be investigated. About 25% of men with a PSA between 2.5 and 10 could have prostate cancer, but it’s often low-grade. For men worried about an elevated PSA, there’s no better place to go for answers than PSA clinic of North Texas.

We Are PSA Experts
Without early warning symptoms, the PSA test is still the best way to detect prostate cancer early. Our world-class prostate cancer specialists help men understand their PSA level, their individual risk for prostate cancer, and how to navigate any next steps that may be necessary.
What is a PSA test?
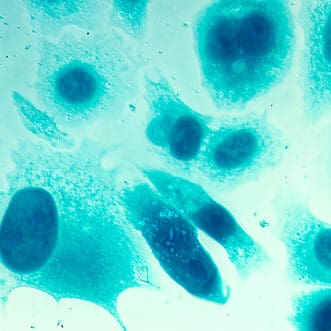
The PSA is a simple blood test that measures the amount of a specific protein—prostate-specific antigen (PSA)—in a man’s bloodstream. PSA is a protein molecule produced not only by prostate cells, but also by prostate cancer cells. PSA protein should remain in the prostate and within ejaculate where it helps liquefy semen and break down other proteins to help sperm live longer. A small number of PSA molecules can leak into the bloodstream, but when a PSA level is higher than normal, it may be a sign of something more serious happening in the prostate.
About one in 41 men will die of prostate cancer. While some criticize PSA screening, it continues to remain the best way to detect prostate cancer.
What is considered a "normal" PSA?
Things to keep in mind before your PSA test.
There are several situations that can lead to a falsely elevated PSA and should be considered before having blood drawn for a PSA test. Men should delay having a PSA test if they have painful urination or a urinary tract infection, engaged in sexual activity with the last 24 hours, or undergone a cystoscopy, catheter insertion or other urinary instrumentation.
Several other factors can cause an elevated PSA, including a man’s age (the prostate naturally grows over time), an enlarged prostate and inflammation of the prostate (with or without symptoms). A simple digital rectal exam (DRE) in the office should not cause any significant rise in PSA. This has been studied extensively, so don’t worry about getting a PSA after a DRE.

It's important to know your “free” PSA level.
The PSA molecule circulates throughout the body in two forms—either bound to other proteins or unbound. The free PSA measures the unbound molecule and is often used by urologists as another helpful indicator for prostate cancer. The lower the percent of free PSA, the higher the risk of having prostate cancer. Patients with free PSA of less than 10 percent can have up to a 56 percent risk of harboring a focus of cancer in their prostates.

Early detection of prostate cancer is vital.
Health Navigator
- Harrison “Mitch” Abrahams, MD
- Jeffrey Charles Applewhite, MD
- Jerry Barker, MD, DABR, FACR
- Paul Benson, MD
- Richard Bevan-Thomas, MD
- Keith D. Bloom, MD
- Tracy Cannon-Smith, MD, FMS
- Paul Chan, MD
- Kara Choate, MD
- Lira Chowdhury, DO, FACOS
- Weber Chuang, MD
- Adam Cole, MD, FS
- M. Patrick Collini, MD
- Zachary Compton, MD
- Adam Hollander, MD
- Patrick A. Huddleston, MD
- Justin Tabor Lee, MD
- Wendy Leng, MD, FPMRS
- Alexander Mackay, MD
- Tony Mammen, MD
- F.H. “Trey” Moore, MD
- Geofrey Nuss, MD
- Christoper Pace, MD
- Jason Poteet, MD
- Andrew Y. Sun, MD
- Scott Thurman, MD
- James Clifton Vestal, MD, FACS
- Keith Waguespack, MD
- Diane C. West, MD
- Keith Xavier, MD, FPMRS
Related News & Information
Life After the Lift (UroLift) is Great!
For many men, an enlarged prostate can make life miserable. The urgent need to go, urinating more frequently than normal, a weak urinary stream, difficulty starting and stopping—they’re all symptoms of BPH. Find out how the UroLift is helping men get their life back.
We Are Your PSA Experts
Call for an Appointment
Prostate Cancer Survivor Paul Moseley Shares His Gratitude for Life
Paul Moseley remembers the day he learned he had prostate cancer in November 2013. “I don’t scare easily, but I was shook,” he admits. “You think you have this big distance ahead of you, and it turns out it could be really short.”

