5005 S. Cooper St.
Suite 250
Arlington, TX 76017
Pelvic Prolapse Feels Pretty Awful

Put Everything Back Where It Belongs!
What Causes Pelvic Prolapse?
Not all prolapse is the same.
There are five types of pelvic organ prolapse—cystocele, enterocele, rectocele, uterine and vaginal vault. Each form of prolapse presents its own challenges.
Cystocele prolapse: Supportive tissue between the bladder and vaginal wall weakens and stretches—allowing the bladder to bulge into the vagina.
Enterocele prolapse: Muscles and tissues that hold the small bowel in place weaken and the small bowel bulges down into the vagina.
Rectocele prolapse: The wall of fibrous tissue that separates a woman’s rectum from her vagina weakens and allows the rectum to bulge into the vagina.
Uterine prolapse: Ligaments and other connective tissue supporting the uterus weaken—allowing the uterus to slide down into the vagina. The vagina may be pulled down and even turn inside out.
Vaginal vault prolapse: Pelvic and vaginal tissues and muscles weaken until the upper portion of the vagina sags and loses its normal shape. It drops down into the vaginal canal or outside the vagina. This type of prolapse may happen on its own or along with a cystocele, rectocele or enterocele prolapse. It happens most frequently in women who have had a hysterectomy.
Health Navigator
- Harrison “Mitch” Abrahams, MD
- Jeffrey Charles Applewhite, MD
- Jerry Barker, MD, DABR, FACR
- Paul Benson, MD
- Richard Bevan-Thomas, MD
- Keith D. Bloom, MD
- Tracy Cannon-Smith, MD, FMS
- Paul Chan, MD
- Kara Choate, MD
- Lira Chowdhury, DO, FACOS
- Weber Chuang, MD
- Adam Cole, MD, FS
- M. Patrick Collini, MD
- Zachary Compton, MD
- Adam Hollander, MD
- Patrick A. Huddleston, MD
- Justin Tabor Lee, MD
- Wendy Leng, MD, FPMRS
- Alexander Mackay, MD
- Tony Mammen, MD
- F.H. “Trey” Moore, MD
- Geofrey Nuss, MD
- Christoper Pace, MD
- Jason Poteet, MD
- Andrew Y. Sun, MD
- Scott Thurman, MD
- James Clifton Vestal, MD, FACS
- Keith Waguespack, MD
- Diane C. West, MD
- Keith Xavier, MD, FPMRS
Related News & Information
You don’t have to live with prolapse.
With physicians certified in female pelvic medicine and reconstructive surgery, Urology Partners offers the latest vaginal, robotic and non-invasive treatment options. Our pelvic organ prolapse specialists help women get back to doing all the things they love without discomfort, worry or embarrassment.
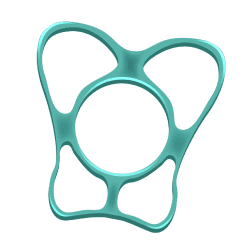
Pessary Devices
This non-invasive approach uses a soft rubbery silicone form known as a pessary. Inserted into the vagina, the pessary gently pushes the prolapsed organ back to its correct position to keep it from bulging into the vagina. Pessaries come in a variety of shapes and sizes, and work for most types of prolapse. Each is custom fit to the woman’s unique anatomy. Pessaries are a good treatment option for older women who are no longer sexually active and women who don’t wish to undergo surgery.
Most women find wearing a pessary very comfortable. Some patients simply wear it during the day, remove it at night to wash it, and then put it back in the next morning. Other women may wear their pessary for up to 10 weeks before they temporarily remove it for washing. Women who want or need help inserting and removing their pessary for washing, can visit the UP office for assistance every 10 weeks or so.
Vaginal Prolapse Repair
This minimally invasive vaginal approach is generally used for less severe cases of prolapse, including cystocele prolapse (bladder bulges into the vagina) and rectocele prolapse (rectum bulges into the vagina). Repair of the prolapse can be made through the vagina (also known as a vaginal colporrhaphy with apical suspension). The repair can be reinforced with tissue from the patient or biologic graft material that’s been treated for safe use in humans.

Robotic Prolapse Repair
When there is a high degree of prolapse involving more than one pelvic organ, a robot-assisted sacrocolpopexy procedure is often required to restore the vagina to its normal position and function. It may also be required in women undergoing a hysterectomy for uterine prolapse who need their pelvic organs suspended.During the procedure, four to six small incisions are made in the abdomen to lift the prolapsed organs and secure them with soft synthetic fabric. Women typically spend one night in the hospital, are advised to take one to two weeks off work, and abstain from sex and other strenuous activities for six weeks.Studies show that five years after surgery, women who undergo a sacrocolpopexy enjoy a 95 to 98 percent success rate.
We Are Your Pelvic Organ Prolapse Specialists
Call for an Appointment

Put Your Prolapsed Organs Back Where They Belong
Women’s bodies endure so much in the normal course of life—pregnancy, childbirth, menopause, hysterectomy, ageing. While the spirit may be resilient, the tissue that holds the pelvic organs in place can have a hard time standing up to the demands. Over time, these tissues stretch and become weak.

