The coronavirus pandemic has taken an unprecedented toll on nearly every aspect of our lives—including one that no one initially saw coming. A sudden and dramatic drop in patients afflicted with non-COVID health issues.
Reports from the frontlines of hospitals have cited a decline in the number of heart attacks and strokes nationally. Not just a small decline, but a drop of up to 60 percent. Are fewer people having heart attacks and strokes? Unlikely. Concern has grown so much that the American Heart Association and American College of Cardiology published a joint statement reminding people that “calling 911 immediately is still your best chance for surviving and saving a life” in the event of a heart attack or stroke.
The National Cancer Institute (NCI) has also sounded the alarm. The Institute conservatively predicts that tens of thousands of additional cancer deaths will occur over the next decade due to missed screenings, delays in diagnosis and a decrease in cancer care caused by the pandemic.
Recently, NCI Director Norman Sharpless, MD, said the pandemic is threatening to undo three decades of “steady and strong progress against death and suffering from cancer, thanks to improvements in prevention, screening, diagnosis and treatment.”
Routine preventative cancer screenings have dropped 90 percent in some systems. Delays in diagnosis along with delayed or modified treatments mean cancer patients are receiving less than optimal care.
Prostate Cancer Screenings Are Down
“All this concern about COVID-19 has made people worry less about more common medical issues—including prostate cancer,” says Adam Hollander, MD, a prostate cancer specialist and surgeon with Urology Partners of North Texas (UPNT). “There’s a big difference in diagnosing prostate cancer early when it’s very treatable and discovering it much later after it’s spread beyond the prostate and is no longer curable.”
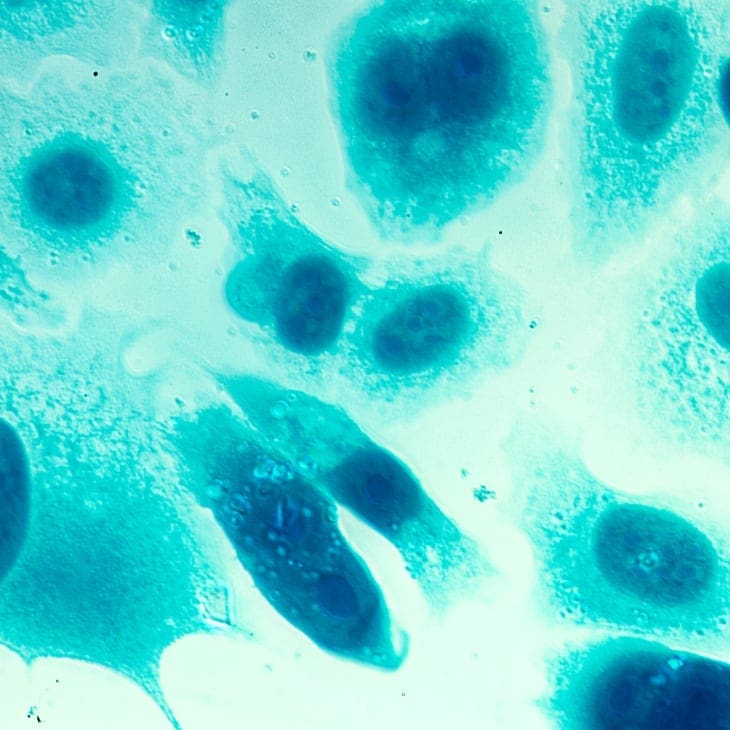
Before the introduction of prostate-specific antigen (PSA) testing in 1991, death rates from prostate cancer were on a steep trajectory. Then they made a dramatic decline—dropping about 39 percent—between 1991 and 2008. Then a controversial recommendation against PSA screening by the United States Preventive Services Task Force (USPSTF) in 2012, derailed progress. Many medical experts fear the USPSTF’s “D” rating has undone much of the gains attributed to routine PSA testing.
Although the last several years have seen a drop in the number of new prostate cancer cases, that doesn’t mean that fewer men have prostate cancer. It means fewer cases of prostate cancer are being diagnosed because fewer men are being tested.
“In many men, we are not finding prostate cancer until it is late-stage or aggressive high-grade cancer—or a cancer that has already spread to other organs,” Dr. Hollander notes. “The whole point of prostate cancer screening is to detect prostate cancer early in healthy men so they can be treated before it becomes life-threatening. With early treatment, the survival rate is 98 percent. Early screening is also important because in its early stage, most prostate cancer doesn’t have symptoms. It doesn’t cause urinary trouble. It doesn’t cause pain. It doesn’t cause weight loss. Screening is the only way to detect prostate cancer early. If it isn’t identified before it causes symptoms, it may be too late.”
A Simple Blood Test Helps Save Lives

This year, more than 33,000 men are expected to lose their battle with prostate cancer. The American Urologic Association recommends men from the ages of 55 to 69 talk with their physician about PSA screening to decide when to begin screening and how often.
“Anyone with a family history should be screened at least five years before the youngest person in their family was diagnosed with prostate cancer,” Dr. Hollander adds. “For example, if your dad got prostate cancer at 48, then you need to be screened at 43. African-American men should begin screening at 55 because they have a higher risk for prostate cancer and a higher risk for having aggressive, high-grade prostate cancer.”
A simple blood test allows men to establish a baseline PSA level that can be monitored over time to ensure it doesn’t creep up into dangerous territory that could indicate prostate cancer.
Levels measuring less than 2.5 are considered within the normal range, but it should be noted that men with a PSA level between 2.5 and 4.0 have a 21 to 23 percent risk for prostate cancer. For men with a PSA level above 4.0, the risk is roughly 27 to 29 percent. The higher the PSA, the higher the risk that the man could be harboring a focus of cancer.
“Our goal with PSA screening is to find prostate cancer early enough, so we can help men have the best possible outcome and live long, healthy lives,” Dr. Hollander explains. “The pandemic shouldn’t get in the way of that. It’s so important for men to take care of themselves now. Many men in their 50s and 60s have urinary or erectile dysfunction issues. Your doctor can evaluate you and make sure there’s nothing more dangerous going on. He or she may be able to help you with your symptoms so you don’t have to simply grin and bear it.”
Finding Ways to Counter the “Fear” Factor

Despite all the good reasons to see a doctor, Dr. Hollander knows an unseen culprit is keeping men away—fear.
“No decision about your health should be changed due to fear,” he asserts. “Men can be reassured that it is safe to come to the doctor’s office. In most cases, it’s probably safer to come in and make sure you are in the clear rather than miss a serious health issue because of fears over COVID.”
Urology Partners has implemented very strict protocols to make sure patients are as safe as possible. Social distancing is observed in all waiting areas. UP staff check in with patients a few days before their appointment to ensure they don’t have any COVID symptoms. Patients are screened for fever and other symptoms when they arrive. The number of people allowed to accompany patients into the clinic is also limited to minimize traffic.
“With all of these protocols in place, it’s probably safer to go to a doctor’s office than go to a grocery store or mall or restaurant where people are gathering and not necessarily being screened adequately,” says Dr. Hollander. “The pandemic protocols will likely be continuing for some time. You can put things off for limited amounts of time, but there are some things that should not be delayed—and that includes seeing your doctor and staying on top of preventive screenings and treatments for any medical issues.”
Have you had a baseline PSA test?
Dr. Hollander and the compassionate physicians at Urology Partners are ready to help you fend off prostate cancer and other urologic issues. Schedule an online appointment, or call 866-367-8768.


